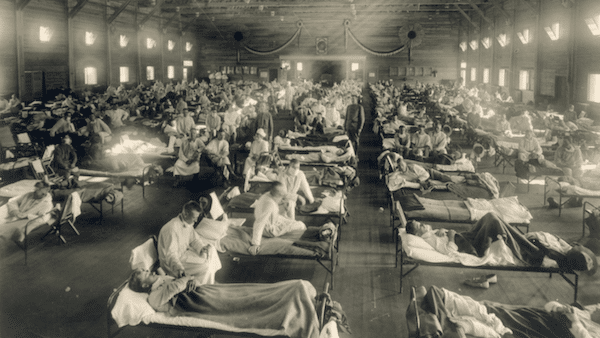
We frequently hear that COVID-19 is the worst pandemic since the 1918 Spanish flu. It is forgotten that the third plague pandemic killed millions in South, South East and East Asia from the 1890s, and continued well after the Spanish flu, to the 1950s. That pandemic killed an estimated 10 million in India alone. I remember my family talking about it, as also numerous stories I read which had plague as their backdrop, and a recent book on the Bombay plague.
So why is this forgotten when we talk about pandemics today? Is the reason for this similar to why the world seems to have forgotten about a host of diseases that still plague the world—diseases that Peter Hotez, a molecular biologist, has called “forgotten diseases” of “forgotten people” in his book? Diseases that the WHO more neutrally terms Neglected Tropical Diseases?
The question is, who has forgotten about such diseases? Certainly not the people, more than a billion of whom live under the threat of contracting them. If we include tuberculosis, malaria, dengue and yellow fever in Hotez’s list of forgotten diseases, the affected people would amount to 65% of the world’s population. It is the well-off countries that believed that infectious diseases did not concern them any more. They were “forgotten” by the rich, as they believed they could keep such diseases out of their countries. The third plague was almost entirely restricted to the colonized world, leaving the colonialists comfortable in their belief that they had now conquered the diseases that affected only the dirty, flea-ridden, rat-infested parts of the world.
The COVID-19 pandemic proves that diseases can strike back and we are only one mutation away from a new infectious disease.
One of the consequences of the belief that infectious diseases are no longer a concern for the rich is the drying up of research funds for developing new medicines for such diseases. Annually, tuberculosis kills 1.5 million people and infects 10 million (WHO’s 2019 TB Report), with India alone accounting for nearly half a million deaths and about 2.7 million infections. Yet the first set of new tuberculosis drugs entered the market after more than four decades! The last three new medicines for malaria, which infects more than 200 million annually, are now 50 years old. Two of these three were developed by the United States Army for its soldiers fighting its colonial war against Vietnamese liberation forces.
In a discussion on Rajya Sabha TV, Venkatraman Ramakrishnan, who won the Nobel Prize in Chemistry in 2009, had said to this author that the current model of developing medicines will not work for infectious diseases for two reasons. One is that drug companies do not see an incentive for developing a drug that cures patients in a few days, for that would mean not needing their drugs any further. The second is that infectious diseases are far more prevalent in poorer countries which cannot pay the prices that multinational drug companies want.
Whether it be medicines for infectious drugs or vaccines—both of which address public health issues—multinationals and big pharma have very little interest in them. That is why infectious diseases have been forgotten by rich countries, who think it is only a problem of the third world; and big pharma, which does not see any profit from such drugs.
The COVID-19 pandemic has laid bare the other contradiction in the capitalist world: ill health provides profits, a healthy population does not. Money is to be made from disease, when people buy pills or have to go to hospitals. Public health was important as long as infectious diseases were perceived to be a threat. As they became “forgotten”, so did public health in the rich countries. In the case of hospitals, what drove the system was either private profit for private hospitals or the same capitalist criteria introduced as “efficiency” in public hospitals.
The capitalist principle of maximizing efficiency was to maximize bed occupancy, a twisted form of “just-in-time manufacturing” introduced by capital to reduce inventories and therefore costs. Reducing beds, equipment and medical staff is, in capital’s terms, “rationalizing” production and increasing “efficiency”.
When the COVID-19 epidemic hit advanced capitalist countries, particularly in the flu season when patient loads are already peaking, they ran into a huge shortage of intensive-care beds, equipment, doctors and nurses. We are not talking about the other problems—the collapse of global supply chains for personal protective equipment (PPEs) and medicines.
What has surprised most observers is the collapse of the health systems in the advanced capitalist countries. Just before the end of January, Forbes magazine “ranked” countries that are “best and worst prepared” to handle the epidemic. The two countries on top in their rankings were the United States and the United Kingdom. Today, the United States has the highest number of infections and deaths in the world while the United Kingdom has already registered the highest number of deaths in Europe. Almost all the countries that Forbes had ranked as best-prepared—the United States and the core European Union countries—have the worst numbers today!
Without getting into why this pandemic has struck the advanced capitalist countries so hard, one issue is clear: these countries may have been prepared to handle normal health issues, and annual flu cases, but they were completely unprepared in their preparations for a novel infectious disease. While East and South East Asia adopted the mask, particularly after their brush with SARS (now SARS-Cov-1) in 2003 and the dangerous H5N1 version of avian flu, the advanced countries have no such experiences. In the less affluent countries, there is a collective memory of infectious diseases—plague, cholera, small pox, polio—and the public health measures that are needed during epidemics. There are even some surveillance and monitoring systems, now matter how weak, to address such issues.
In the United States, the threat of a new infectious disease is not even a part of the collective psyche of the people. That is why, with a lockdown imminent, guns and ammunition were in as high demand as medicines and food. The threat was clearly other people and not a virus or germs.
Amit Sengupta had written extensively in Newsclick and elsewhere about the contradiction between capital and people, between the greed for profit (and profiteering) and people dying for lack of medicine. He wrote, “Unethical behavior of healthcare providers is directly linked with the fact that if care is linked to profit, more ill health means more profit! … Governments, not markets, can ensure that health systems address the needs of the poorest and the most marginalized.”
It is not an accident that COVID-19 deaths in the advanced countries are concentrated among immigrant communities, the poor, and the socially excluded. It is the African American and Hispanic populations in the United States which are seeing a disproportionately high number of deaths and infections. It is the immigrant areas in the European Union and United Kingdom that are again seeing much larger numbers of deaths and infections. But diseases are also levelers; the poor and the excluded may suffer more, but it will not spare the rich either. And this time, the rich countries, who thought they had left their infectious past behind, are beginning to understand that in a globalized world they will not escape either.
This is the question that Amit Sengupta posed in the last Peoples Health Assembly in Dhaka in 2018. What happens when the hunger of capital enters the belly of the beast? When this hunger enters those countries that Forbes thought were best prepared to face the pandemic?
The novel virus—SARS-Cov-2—has brought the old challenge of disease back to the list of existential challenges that humanity faces. We know that the race between microbes and us is a continual battle. As we evolve our defense, they develop their offense. We know that we upset the global ecological balance—climate change—at our peril. What is not understood widely—except in the left—is that the biggest obstacle to charting a path for humanity that lets us address these challenges is capitalists and their greed.
Pandemics have not only spread death and destruction, they have also changed societies in fundamental ways. No, the world will not look the same once the COVID-19 pandemic is over with herd immunity, either through vaccination or infections. But will it lead society to confront capital’s greed against people’s lives? That is the challenge before all of us; this is how history will judge us.