Last April, as the coronavirus pandemic took off, I ventured into an analysis of its health and economic impact. As I said at the time,
It is a risky thing to start analysing the COVID stats and coming up with some conclusions at this still early stage of the pandemic. It is even riskier for an economist to delve into areas beyond his or her supposed expertise. But after looking at myriads of articles, heaps of data and lots of presentations by people who ought to know what they are talking about, I cannot resist putting my dollar on the table.
I think it is worth rereading that post, because, looking back, I think my analysis has held up pretty well six months later. At the end of that post, I concluded the following things. First, COVID-19 has a much higher mortality rate than flu. Second, without containment it would have increased the annual mortality rates of most countries by over 80%. Third, containment has worked in driving down potential deaths from millions to hundreds of thousands (unfortunately over a million so far). Fourth, because most governments were unprepared and lacked sufficient healthcare facilities, they were forced into varying degrees of lockdowns, bringing the world economy to a standstill. Fifth, the more severe the lockdown and the more health facilities available means generally that there will be fewer deaths; and sixth, the ‘lockdown lite’ approach risks more deaths without offering a stronger economy as a trade-off.
Now I am going to reconsider each of these conclusions in the light of what we now know–again with a fair degree of humility about what we do not know.
First COVID and flu. The debate continues to rage among epidemiologists and other ‘experts’ about whether COVID-19 has a higher mortality rate than annual flu. The so-called Barrington declaration of one group argues that COVID is no worse than flu and can be combated without draconian and damaging lockdowns, perhaps by allowing the young and fit to get the virus while isolating the old and sick, so that ‘herd immunity’ is reached (where sufficient people become immune that the virus abates). In response, most experts refute that approach. They argue that COVID is much more dangerous than flu, that herd immunity will never be reached before millions die and so the pandemic requires containment, short of an effective vaccine and maybe even then.
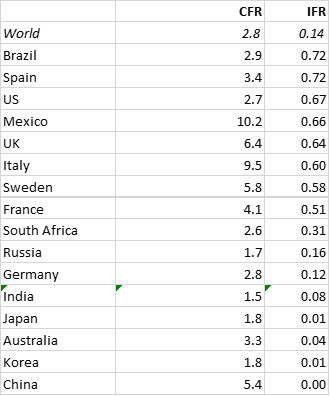
The infection fatality rate (IFR) measures the percentage of the population that dies from a disease. It differs from the case fatality rate (CFR), which measures the percentage of those who die from those cases confirmed as having contracted a disease. The distinction is important, because as we now know, due to poor testing and the fact that many can catch COVID without exhibiting any symptoms or reporting such for medical help, the number in the population who have been infected is much higher than those confirmed as COVID cases.
The IFR for flu averages each year anything between 0.1% and 1%. What about COVID? We don’t really know. We have data for the CFR for COVID, but by how much does the CFR differ from the IFR? The difference will vary among countries because of the age demography of the population (young people get less symptoms); the testing and tracing efficacy operating; the degree of lockdown and social distancing etc. The World Health Organisation reckons that about 10% of the global population may have been infected so far. Some micro studies of antibodies in a population group suggest higher and lower percentages. For example, it has been estimated that despite Sweden’s ‘lockdown lite’, probably only 6% of Swedes have been infected so far.
What we do know are the number of cases reported as being COVID-based and the number of deaths confirmed as due to COVID by each country’s medical authorities. Of course, the reliability of these records varies from country to country, with different criteria and levels of record varying. Nevertheless, I think we can use the data that we have from official sources globally to make some judgements on the death risk from COVID relative to flu.
So I have taken the latest official figures for COVID cases and deaths for various countries and from this worked out the CFR for each. Then I have assumed a 10% infection rate for each country’s population (probably too high) to obtain country IFRs.
This is what I calculated.
You can see that the global IFR (based on 10% infected) is only 0.14, still above the highest IFR for annual flu, but not far above. However, if you look at the some of the major infected countries globally, you can see that the IFRs are generally around 0.6-0.7, which is pretty much in line with the consensus estimate by the scientific experts. And if that is right, then COVID is at least six to seven times more deadly than annual flu. The reason the global IFR is so much lower is because many high population countries have been infected less; because many of these countries have a much greater proportion of young people than in Europe or the US; and because medical treatments and hospital care have got much better at saving lives.
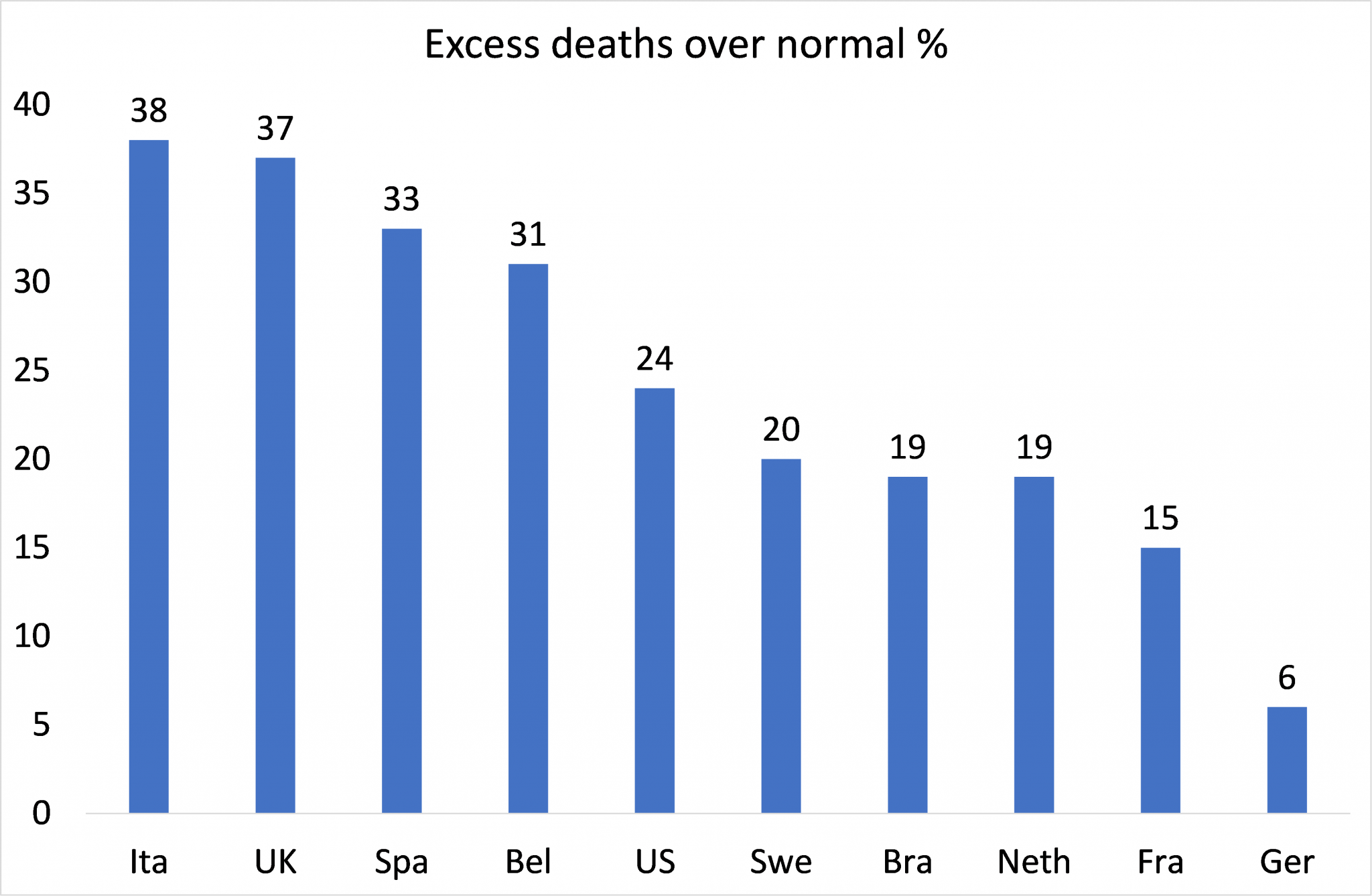
The other piece of evidence that supports the view that COVID is more deadly than annual flu are the excess deaths reported for this year in various countries compared to the average. Only this week, the U.S. Center for Disease Control and Protection (CDC) has found that 300,000 excess deaths were recorded in the U.S. this year–66% of which are accounted for by the official coronavirus death toll of around 220,000. Usually, between the beginning of February and the end of September, about 1.9 million deaths are reported in the U.S. This year, it is closer to 2.2 million–a 14.5% increase. While the remaining 100,000 deaths may not be people who had contracted coronavirus, these deaths may be indirectly related to the pandemic: a heart attack victim, for example, who might not have been able to get treatment because hospitals were overwhelmed.
By whatever measure the pandemic’s grimmest accounting is computed, the UK’s death toll–and particularly England’s—remains among the highest in the world. By its headline figure, 38,524 people in England have died within 28 days of a positive COVID-19 test, but this rises to 42,672 if you extend the cutoff to 60 days, according to the UK’s coronavirus dashboard. The Office for National Statistics, meanwhile, has tallied 50,642 death certificates mentioning COVID-19 up to October 2, and, if you begin counting on March 6, the day that the 100th positive case was recorded, 56,537 deaths in excess of the average for the same period in the past five years. This figure includes deaths from all causes, including COVID-19.
Excess deaths over ‘normal’ range from 6% in Germany to nearly 40% in Italy and the UK.
Finally, on the health aspects of COVID-19, it is becoming clearer that this virus can leave long-lasting damage to people who catch it, but do not die. What is called ‘long COVID’ can cause disorders in brain, lungs, heart, gut, liver and skin that often persist, something that is not the case with flu.
My general conclusion from this evidence is that COVID-19 is not the same as flu; it is much more dangerous and so the call by the majority of scientists that this pandemic had to be contained and not just ignored or merely ‘mitigated’ was correct. But as I said in my April post: “containment can mean many things. It can mean from total lockdown of all economic and social movement and activity to more relaxed measures, down to simply testing everybody for the virus, isolating and quarantining those infected and shielding the old, while hospitalising those with severe conditions. If a country had full testing facilities and staff to do ‘contact and trace’ and isolation; along with sufficient protective equipment, hospital beds including ICUs), then containment along these lines would work–without significant lockdown of the economy.”
Looking back, my suggestion that efficient, well-funded and resourced public health systems and methods might have been enough to avoid heavy lockdowns may have been optimistic. And that’s not just because many countries were not prepared or able to provide the facilities and resources to do that. Even in those countries with good health systems and well applied containment plans, (eg China, Korea, Germany) there was probably still the need for a lockdown and social distancing. Lockdowns worked when applied properly. China is the most exceptional example of a high-level lockdown in one large province. New Zealand applied a high-level lockdown from day one and reduced deaths to the bare minimum.
South Korea acted quickly, taking advantage of legislation passed in response to the 2012 Mers crisis that allows for extensive surveillance of its citizens during an infectious disease outbreak. A comprehensive contact-tracing operation was put in place, partnered with a rapid expansion of testing. On March 20, South Korea was carrying out 100 tests for every positive one that came back, the same day it recorded its 100th death. It took Italy three more months and 34,000 deaths to reach the same testing levels.
Unfortunately, lockdowns could not be applied effectively in many countries of the ‘Global South’. Public health systems were inadequate or non-existent. Enforcement of proper social distancing proved difficult, as many people are employed in the informal economy, without a safety net that would allow them to apply for Covid-related government handouts. They often depend on daily wages for their evening meal. In India, high levels of urbanisation, coupled with inadequate housing and sanitation, as well as a large informal labour force, formed perfect conditions for the virus to wreak havoc, especially in the country’s mega-cities and slums.
The Swedish authorities opted to what might be called ‘lockdown-lite’, with restrictions only on mass gatherings and relying on voluntary social isolation. But even though Sweden has a relatively low level of urbanisation, is away from continental Europe and has a population prepared to apply social distancing with some discipline, the cumulative COVID death rate in Sweden is not far short of Italy and Spain, and is way higher than its Nordic neighbours, Denmark, Finland and Norway, which did impose early and much stricter lockdowns.
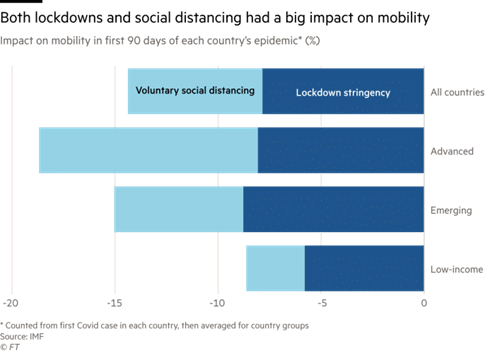
But it is not just lockdowns. According to the IMF, mobility and economic activity dropped from April to June just as much from people deciding voluntarily to stay at home and social distance as to government lockdown restrictions.
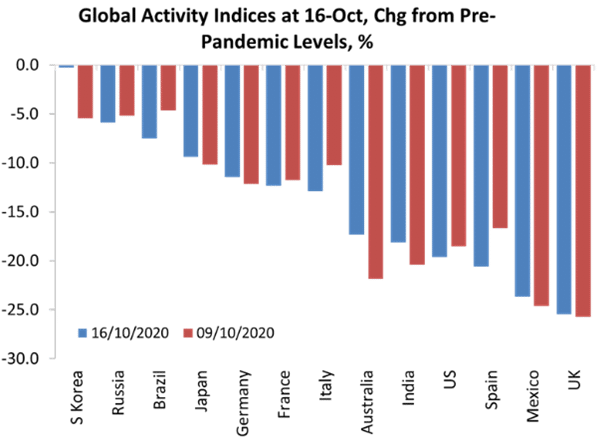
Of course, lockdowns have been devastating for economic activity and people’s livelihoods. I have highlighted the economic impact of the lockdowns and the ensuing pandemic slump in various posts. But now it has become clear that those countries that did impose early lockdowns last March and introduced effective test and trace systems and massive medical support were able to come out of those lockdowns earlier and thus start to revive the economy.
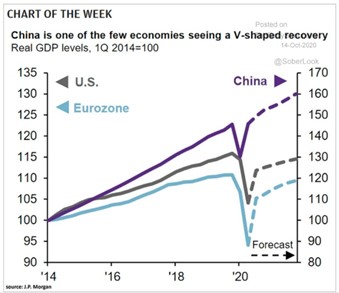
The best example is China, where COVID first started. A draconian lockdown was imposed in Wuhan to isolate the disease from the rest of country. By April that lockdown was lifted and combined with mass testing and tracing and community cooperation on social distancing, China was able to restart its economy quickly. While the major capitalist economies of the world are struggling to recover amid a new outbreak of infections, the so-called ‘second wave’, and are waiting desperately for a vaccine to provide the ‘silver bullet’ to deal with the virus, China’s economy is now growing again.
It is achieving a V-shaped recovery, while the major capitalist economies are languishing in a long-term ‘reverse square root’ recovery, one where real GDP, employment and investment will struggle to return to pre-COVID levels for years, if at all.
What the experience of the last six months tells us is, contrary to the views of the ‘contrarians’ and ‘libertarians’ and many governments (both right-wing and supposedly left), there is no trade-off between lives and livelihoods. Containment including lockdowns can save lives and control the disease and thus enable people to get their livelihoods back–assuming their bosses have not sacked them anyway.
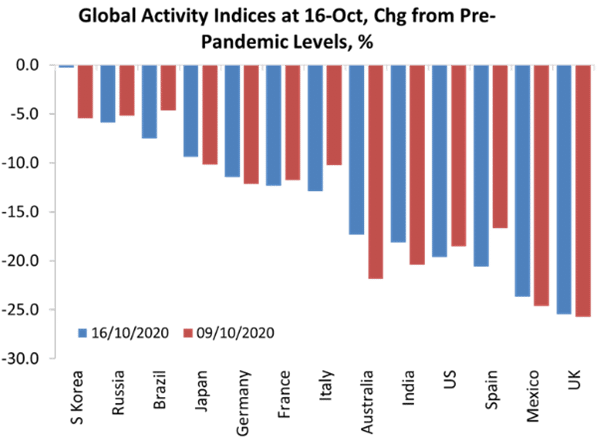
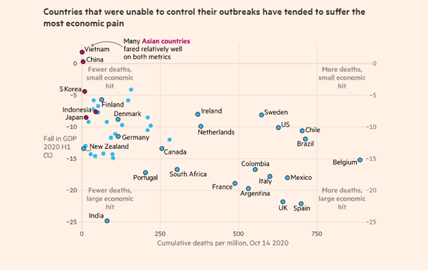
Countries that had invested heavily in good health systems, applied effective test and tracing and yes, early lockdowns, have saved lives AND reduced the damaging economic impact of the pandemic (they are the countries in the top left of the graph below). Those countries that have neglected or privatised their health systems, have failed to test and trace properly and have vacillated over lockdowns in order to ‘save the economy’ have ended up with more deaths and more damage to their economies (bottom right of the graph). Note the contrast between China and India, or China and the UK.
The sixth conclusion from my post last April has been proven right.