Part Two of a multi-part article on the causes and implications of global capitalism’s descent into an era when infectious diseases are ever more common. My views are subject to continuing debate and testing in practice. I look forward to your comments, criticisms, and corrections.
[Part 1] [Part 3] [Part 4] [Part 5] [Part 6]
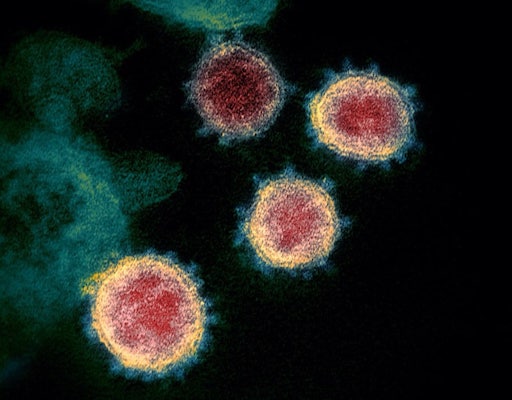
A question that goes unasked in most accounts of the COVID-19 pandemic is why now? Why has a virus that for centuries resided peacefully in a wild animal in rural China suddenly attacked millions of humans around the world?1
For a potentially deadly virus to cause actual disease, conditions must exist for it to infect a plant or animal and multiply. And for a disease to become an epidemic or pandemic, conditions must exist for it to spread rapidly to others. Epidemics and pandemics are simultaneously micro-biological and macro-ecological2—they emerge and spread through interaction and conflict between biological change and social change.
To understand why new viral diseases are multiplying now, we focus first on the relentless evolution of Earth’s smallest and most numerous biological entities.
+ + + + + +
If you ask most people what viruses are, they’ll say something about germs and disease. Indeed, until recently that was how most scientists viewed them: in 1977 the famous biologists Jean and Peter Medawar wrote that a virus is “simply a piece of bad news wrapped up in protein.” No one could see a virus before the invention of the electron microscope in the 1930s, and unless it caused disease, scientists didn’t know to look for it. For decades, viruses were classified by their appearance and their impact on human health.
Only in this century has automated genetic analysis enabled the rapid identification of large numbers of viruses, causing a revolution in virology. In study after study, scientists are discovering thousands of previously-unknown viruses at a time—so many that efforts to catalog them have trouble keeping up, and we have no idea what (if anything) most of them do.
The figures are mind-boggling. Can anyone truly grasp numbers like the estimated 1031 individual viruses on Earth—10 million times as many as there are stars in the universe? Every liter of ocean water contains about 100 billion viruses, and wind-borne dust carries some 800 million viruses to every square meter of the earth’s surface, every day. There are about a trillion viruses in your body at any given time—some infect your human cells, some infect the millions of bacteria we all carry, and some are just passing through on your food or breath.
They are, as evolutionary biologist John Thompson writes,
in many ways the most successful lifestyle on earth.3
Viruses are, by far, the most abundant organic entities we know of; in fact, they are probably more common than all other forms of life combined… Every ecological niche in which life can be found has been penetrated by the virosphere. Over 100 million types of viruses infect all species of living beings, including animals, microbes, and plants.4
Most viruses are specialists that can only infect particular species of microbes, plants, or animals—and usually only specific kinds of cells in specific species. Rabies, for example, initially infects muscle cells of some mammals, then attacks their brain cells. Ebola viruses target cells in human livers and immune systems, and the linings of our veins and arteries. Coronaviruses infect cells in human respiratory tracts, some causing mild cold symptoms and others causing SARS or COVID-19.
Viruses play major roles in the biogeochemical cycles that define and drive the entire Earth System. Some viruses kill billions of single-celled organisms in the oceans every day, sinking (and eventually recycling) millions of tons of organic carbon. About one-quarter of fixed carbon passes through such virus-driven processes, and five percent of the oxygen you breathe comes from virus-stimulated photosynthesis in the oceans. Many viruses co-exist in permanent symbiotic relationships inside the cells of plants and animals, killing harmful bacteria, stimulating production of essential chemicals, aiding digestion, and much more. About 8% of the human genome is DNA that originally came from various viruses.
But in this article I focus on the small minority, a fraction of a percent of all virus species, that can cause disease in humans and other animals. Two biological characteristics, common to all viruses, make these potential pathogens particularly dangerous.
1. Viruses cannot reproduce on their own. Viruses are unlike any other form of life—indeed, there is an ongoing debate about whether they are alive at all. They have no metabolic systems of their own, no source of energy to do anything at all. This is life (if that word applies) stripped down to a handful of RNA or DNA instructions for making copies of itself. It can only reproduce by entering a living cell and hijacking its reproductive machinery. When it does so, hundreds or thousands of copies can be manufactured and released into the environment in a few hours.
That reproduction process can cause disease either by preventing cells from performing essential functions for the larger organism, or by provoking the host’s immune system into over-reaction, or by some combination of those. As virologist Marilyn Roossinck writes:
If we imagine that viruses have a goal, it is simply to make more of themselves. They are not driven to cause disease or to do good; they just want to make more viruses. Sometimes, in this drive to reproduce, they benefit their hosts, and if that happens there may be strong selection to maintain the relationship. At other times they accidentally cause harm to their hosts, especially if they and their host have a new relationship that has yet to be honed through adaptation and evolution. Ultimately, a virus will adapt anything that furthers its cause to reproduce.5
Despite the language of “goals,” viruses do not in any sense seek out new cells to infect. When not in cells, viruses are inert, unable to do anything at all. Only accidental contact with appropriate cells allows them to resume reproducing, but because there are millions of them, chances are that some will infect new cells and resume reproduction.6
2. Viruses constantly evolve as they reproduce. Unlike cells, viruses don’t reproduce by dividing—instead they force the host cell to create the necessary proteins, and then to assemble them into copies of itself. In contrast to DNA, with its famous “double helix” structure that identifies and corrects copying errors when a cell divides, the genetic material of most viruses is RNA, which has no such error-correcting ability. On average, there is one mistake, or mutation, in every copy of an RNA virus.7 If two kinds of viruses infect the same cell, they may shuffle their genes, creating hybrids. Most mutations and gene exchanges weaken or disable the virus, but any that confer a survival advantage will tend to spread through the virus population.
This churn of genes creates infinite opportunities for new viruses and viral particles to evolve and pass through diverse life forms. Thus, over several trillions of generations, once-cousins create progenies that are progressively more distinct from one another.8
In essence, the combination of copying errors and Darwinian natural selection leads to large numbers of simultaneous experiments in viral evolution. As Marxist biologist Richard Levins warned three decades ago, constant evolutionary change gives microbial pathogens a significant advantage over medical science.
The genetic makeup of pathogen populations… shifts readily, not only in the long run but even in the course of a single outbreak and within a single host during a bout of illness. There are strong opposing demands on the pathogen’s biology to select for access to nutrients, to avoid the body’s defenses and exit to a new host. Variations in a body’s state of nutrition, its immune system, the presence or absence of other infections, access to treatment, the treatment regime and conditions of transmission all push and pull the genetic makeup of pathogen populations in different directions. This means that we constantly see new strains arising, new strains that differ in their drug and antibiotic resistance, clinical course, virulence, and biochemical detail. Some even develop resistance to treatments that have not yet been used if these threaten the survival of the pathogens in ways similar to old treatments.9
A virus that kills its host will go extinct unless it has can infect another before the first host dies. Usually such movement only occurs within a species, but zoonotic infections can occur when a virus jumps or “spills over” from animals to humans. When that happens, a virus that was harmless in the original species may cause serious illness, even death, in the next. But a virus cannot infect a new species if appropriate conditions for species-switching don’t exist. Ecologist Jaime García-Moreno explains that the physical and biological barriers to moving from one species to another have made such shifts relatively rare.
Pathogens are often confined to one host species (or to a group of related species), and so, in spite of being continually exposed to multiple pathogens that have other species as hosts, most of these cannot and do not infect people; those that manage rarely cause disease in humans and almost always lead to dead-end infection chains…
It is clear that the mere appearance of a new pathogen is insufficient to cause a new disease, because there are many factors that end up determining whether a pathogen can infect a potential host and whether the infection can become self-propagating—host distribution, pathogen release from the host and survival, human (or other new host) exposure, or immune response to name just a few. We are exposed daily to multiple viruses, but only very few have evolved the mechanisms to cause a successful infection cycle in human beings.10
Nevertheless, over the centuries many viruses have made the jump. Some early hunters undoubtedly contracted deadly diseases from the blood of animals they killed, butchered and ate, but their societies were too small for the pathogens to persist as human diseases. That changed with the Neolithic revolution, when livestock farming brought large numbers of humans into frequent direct contact with animals. Livestock farming created a “a bonanza for our microbes… when we domesticated social animals, such as cows and pigs, they were already afflicted by epidemic diseases just waiting to be transferred to us.”11
But just crossing over to human hosts didn’t ensure long-term viral success. To continue as human pathogens, a virus must be able to move to uninfected humans before the infected ones die or develop immunity. That condition was met by the formation of large settlements and cities that accompanied the adoption of agriculture. Large numbers of people living in close to proximity provided ideal environments for animal-based pathogens to spread and adapt to human biology.
Since Neolithic times, hundreds of viruses have successfully moved from animals to humans—first infecting local communities and then spreading to others in the bodies of soldiers and traders. In some cases—the European invasion of the Americas is a particularly horrendous example—this caused pandemics that killed millions of people who had not developed immunity.
Most of the infectious diseases that now afflict humans—including viruses, bacteria, fungi, and parasites—originated in wild and domestic animals. A report published in 2020 found that “across the globe, the 13 most common zoonoses were most impactful on poor livestock workers in low-and middle-income countries and have caused an estimated 2.4 billion cases of illness and 2.7 million deaths in humans per year.”12 Those numbers were almost immediately made obsolete by COVID-19.
The number of microscopic pathogens we now face is unprecedented in our history, and more are coming. As a blue-ribbon scientific panel told the U.S. government in 1993:
It is unrealistic to expect that humankind will win a complete victory over the multitude of existing microbial diseases, or over those that will emerge in the future… Microbes are ranked among the most numerous and diverse of organisms on the planet; pathogenic microbes can be resilient, dangerous foes. Although it is impossible to predict their individual emergence in time and place, we can be confident that new microbial diseases will emerge…
Although the odds are low that a randomly chosen organism will become a successful human pathogen, the great variety of microorganisms in nature increases those odds… Co-evolution of pathogens and their animal and human hosts will continue to be a challenge to medical science because change, novelty, or ‘newness’ is built into such relationships…13
Radical environmental changes, driven by capitalism’s inexorable drive to grow at all costs, have weakened natural barriers against the emergence of novel pathogens, and multiplied opportunities for aggressive viruses to infect humans. As a result, we are seeing the emergence of more zoonotic diseases, and can expect that global pandemics will increasingly characterize the Anthropocene.
To be continued…
References:
- ↩ Some readers have asked about claims that the virus came from a Chinese laboratory. Research into the exact origin is ongoing, but the evidence for animal origin is very strong, while the evidence for a lab link is virtually non-existent. See: www.msnbc.com
- ↩ Chuăng, Social Contagion: And Other Material on Microbiological Class War in China (Chicago, IL: Charles H. Kerr Publishing Company, 2021), 24.
- ↩ John N. Thompson, Relentless Evolution (Chicago: Univ. of Chicago Press, 2013), 113.
- ↩ Anne Aronsson; Fynn Holm, “Multispecies Entanglements in the Virosphere: Rethinking the Anthropocene in Light of the 2019 Coronavirus Outbreak,” The Anthropocene Review 9, no. 1 (2022): 26.
- ↩ Marilyn J. Roossinck, Viruses: A Natural History (Princeton: Princeton University Press, 2023), 64.
- ↩ Dorothy Crawford, Viruses: The Invisible Enemy, 2nd ed. (Oxford: Oxford University Press, 2021), 14.
- ↩> Roossinck, Viruses, 138.
- ↩ Pranay G. Lal, Invisible Empire: The Natural History of Viruses (Gurugram, Haryana, India: Penguin/Viking, 2021), 41.
- ↩ Richard Levins, “When Science Fails Us,” International Socialism, September 1996.
- ↩ Jaime Garcia-Moreno, “Zoonoses in a Changing World,” Bioscience 73 (n.d.): 712.
- ↩ Jared M. Diamond, Guns, Germs, and Steel: The Fates of Human Societies (New York: Norton, 1999), 205—6.
- ↩ Md. Tanvir Rahman et al., “Zoonotic Diseases: Etiology, Impact, and Control,” Microorganisms 8, no. 9 (September 12, 2020): 1405.
- ↩ Institute of Medicine, Emerging Infections: Microbial Threats to Health in the United States, ed. Joshua Lederberg, Robert E. Shope, and Stanley C. Oaks, 3. (Washington, DC: National Acad. Press, 1993), 32, 44.